ISBAR in Hospice: Clearer Calls, Faster Comfort
A Good Call Can Prevent a Bad Death
Calls carry emotion, not just data. Time is short, and clarity is essential.
“ISBAR was born from nuclear urgency. In hospice, we face human urgency.” — Brian H. Black, D.O.
ISBAR began as a safety tool on nuclear submarines to ensure clear communication, later adopted in aviation and medicine to standardize high-stakes patient care. Its structure proved so effective it spread through ICU, surgery, and hospice—where human urgency replaces technical urgency (Burgess et al., 2020; Schmidt et al., 2019).
Hospice ISBAR isn’t a phone script. It’s a discipline that converts anxiety into clarity, steadies teams, and protects dignity when minutes matter.
In the pause between uncertainty and decision, your next words decide whether the night steadies or spins. In hospice, clarity isn’t optional for care—it is the care.
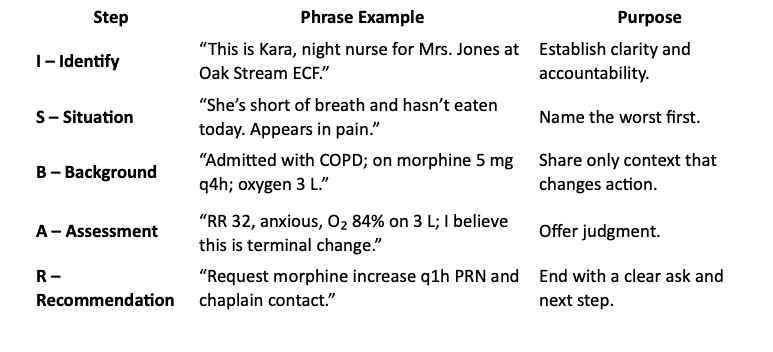
Before You Dial: The 30-Second ISBAR Checklist
Before you call
Confirm goals and code status.
Identify the primary concern.
Have meds, allergies, and vitals ready.
Steady your voice—tone sets temperature.
Repeat orders verbatim before ending.
Perfection isn’t the goal. Precision with compassion is.
(CMS §418.56(c) requires effective IDG communication; ISBAR supports that standard.)
Worst First: Identify the Urgency
Lead with what threatens comfort now.
Consider these two versions of the same hospice call:
Story-first call (inefficient):
“I’m seeing John today. He is a sweet guy, but more restless lately and less talkative. Triage called to get a visit scheduled because family is worried... I drove there today and he has definitely declined... His O₂ is 84%.... What do you want to do?”
Worst-first ISBAR (idealized):
“This is Ashley after hours nurse. John Smith is 94, somnolent, ashen color. He is on service for COPD and CHF. RR 34, O₂ 84% on 3 L. PPS dropped to 20. No edema. PRN morphine 5 mg wears off after 2 hrs. Appears to be transitioning. Recommend increase to q1h PRN and notify chaplain.”
The first drifts. The second directs. This change in structure to ISBAR leads to rapid symptom control and allows the family to gather for a final goodbye, demonstrating how structured communication can directly impact patient comfort and family experience.
Great calls:
State the threat.
Give the facts that change action.
Offer a next step.
ISBAR does all three—fast.
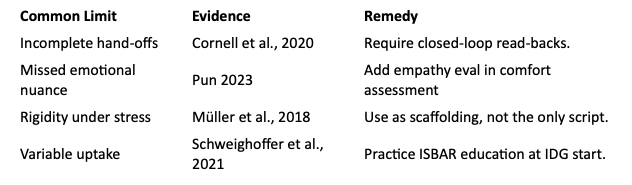
ISBAR Evidence at a Glance
Benefits:
Reduces handoff errors and medication discrepancies by ≈30% (Pinto et al., 2025; Müller et al., 2018).
Improves detection of psychosocial & spiritual needs (Pinto et al., 2025).
Raises family comprehension and satisfaction (Izumi et al., 2020; Ryan et al., 2022).
Speeds team response and cuts after-hours escalations (Schweighoffer et al., 2021).
Prevents adverse events and failed hand-offs (Müller et al., 2018; Burgess et al., 2020).
Supports CMS compliance and CAHPS scores (Joint Commission, 2007).
Works by phone, bedside, or note.
Limits & Fixes:
“Used with judgment, ISBAR becomes fluency—not just formula. Used rigidly, it misses the moment.” — Brian H. Black, D.O.
Beyond the Phone: Why It Matters
Use ISBAR for nurse-to-provider calls, team hand-offs, IDG updates, and debriefs.
“Name the worst first. Say what you believe. Offer the next step.” — Brian H. Black, D.O.
Over 80 % of sentinel events trace to communication failure (Joint Commission, 2007).
In hospice, that means families may miss moments they can never reclaim.
Clarity builds trust across the power gap. It lets the clinician see the scene.
Across the IDG
RN: Lead with symptom + time course; confirm PRN window.
SW/Chaplain: Add emotional or spiritual insight in A.
Aide: Report new functional loss or barrier.
NP/Physician: Turn the ask into a clear, time-bound order.
All: Read back key orders before hanging up.
Each clear call shortens suffering and fulfills §418.56(c).
Used well, ISBAR is teamwork in real time.
3-2-1 Summary
3 Key Insights
ISBAR structures urgent hospice calls.
“Worst first” prevents delay and keeps focus on comfort.
Stating judgment builds trust and guides decisions.
2 Actionable Ideas
Practice a 30-second ISBAR at your next team huddle.
Open your next IDG with a 2-minute ISBAR drill.
1 Compassionate Call to Action
Speak with clarity and courage. Teach ISBAR today. Use it tonight.
Track clarity like comfort—monitor call response times, repeat-call rates, and CAHPS communication scores.
Glossary
Hospice ISBAR — Structured call format adapted from nuclear safety to hospice. Begins with urgency, states judgment clearly, and ends with a goal-aligned next step. Creates shared language that speeds decisions and builds confidence.
Worst First — Communication principle leading with the highest-risk concern before any background. Keeps focus on what threatens comfort now.
Bibliography
Burgess, A., van Diggele, C., Roberts, C., & Mellis, C. (2020). Teaching clinical handover with ISBAR. BMC Medical Education, 20(Suppl 2), 459. https://doi.org/10.1186/s12909-020-02285-0
Cornell, P., Gervis, M. T., Yates, L., & Vardaman, J. M. (2020). Impact of SBAR on nurse–physician communication and patient safety: A systematic review. Journal of Hospice & Palliative Nursing, 22(1), 13–20. https://doi.org/10.1097/NJH.0000000000000615
Izumi, S., Noble, B. N., Candrian, C. B., & Nussbaum, J. F. (2020). Hospital-to-hospice transitions: Gaps and opportunities. Journal of Palliative Medicine, 23(7), 900–906. https://doi.org/10.1089/jpm.2019.0524
MacDougall-Davis, S. R., Kettley, L., & Cook, T. M. (2016). The “Go-Between” study: SBAR versus traffic lights in simulation. Anaesthesia, 71(7), 764–772. https://doi.org/10.1111/anae.13457
Müller, M., Jürgens, J., Redaèlli, M., Klingberg, K., Hautz, W. E., & Stock, S. (2018). Impact of the communication and patient hand-off tool SBAR on patient safety: A systematic review. BMJ Open, 8(8), e022202. https://doi.org/10.1136/bmjopen-2018-022202
Pinto, F., Roberto, P., Ferrario, L., et al. (2025). Using “Situation–Background–Assessment–Recommendation” in palliative care to enhance handover quality and nursing practice: A mixed-method study. Journal of Clinical Nursing, 34(1), 117–127. https://doi.org/10.1111/jocn.17537
Pun, J. (2023). Nurses’ perceptions of the ISBAR handover protocol and its relationship to the quality of handover: A case study of bilingual nurses. Frontiers in Psychology, 14, 1021110. https://doi.org/10.3389/fpsyg.2023.1021110
Ryan, R. E., Connolly, M., Bradford, N. K., et al. (2022). Interventions for interpersonal communication about end-of-life care between health practitioners and affected people. Cochrane Database of Systematic Reviews, 7, CD013116. https://doi.org/10.1002/14651858.CD013116.pub2
Schmidt, T., Kocher, D. R., Mahendran, P., & Denecke, K. (2019). Dynamic pocket card for implementing ISBAR in shift handover communication. Studies in Health Technology and Informatics, 267, 224–229. https://doi.org/10.3233/SHTI190831
Schweighoffer, R., Blaese, R., & Liebig, B. (2021). Organizational determinants of information transfer in palliative care teams: A structural equation modeling approach. PLoS One, 16(6), e0252637. https://doi.org/10.1371/journal.pone.0252637
The Joint Commission. (2007). Sentinel event alert, issue 35: Preventing communication failures. https://www.jointcommission.org/resources/patient-safety-topics/sentinel-event/sentinel-event-alert-issue-35-preventing-communication-failures/
National Comprehensive Cancer Network. (2025). Palliative Care (Version 1.2025). https://www.nccn.org/professionals/physician_gls/pdf/palliative.pdf